Schizophrenia İn Women
Schizophrenia in women is widely misunderstood—and misdiagnosed
Not enough is known about how the disease affects women, who are more likely than men to be overlooked—and more likely to develop the disease in midlife.

Long considered the stepchild of healthcare, mental illnesses such as depression and anxiety have increasingly become more visible and better understood. The same cannot be said of schizophrenia, especially in women.
Part of the problem is that schizophrenia, a severe mental illness characterized by hallucinations, delusions, and incorrect thinking, was previously thought to be rare. Official figures put the rate at about a half of one percent. But new research published this summer by the nonprofit Research Triangle Institute shows that to be a vast undercount. Some 1.6 percent of American women are now recognized to have a lifetime history of a schizophrenic disorder. For men, often the face of the disease, the figure is only slightly higher at 2 percent.
“Schizophrenia deserves much more attention,” especially in women, says Deanna Kelly, a psychiatrist and researcher at the Maryland Psychiatric Research Center at the University of Maryland. Inadequate research over the decades means the differences between women and men with the disease are not well understood, which can lead to less effective care, she says.
Numerous questions remain about the disease in women, says Katy Thakkar, a psychologist at Michigan State University who recently examined some of the gaps. For example, the first schizophrenic episode tends to occur in males during their teenage years whereas the disease hits females three to five years later; some women first succumb around menopause.
Doctors have long believed that women with schizophrenia fare better than men, but that’s not necessarily the case. While they are less likely to commit suicide, a study of people in Finland published in the journal Nature found women are slightly more likely to be hospitalized for their illness in the 10 years following diagnosis.
Getting the right diagnosis
Disparities begin right at the start: Women with schizophrenia are more prone to being misdiagnosed.:max_bytes(150000):strip_icc()/what-are-the-symptoms-of-schizophrenia-2953120-e15ca22957ec44ff8969cf9b8ac24568.jpg)
This is something Analisa Chase knows all too well. The 31-year-old autism therapist in Takoma, Washington, has schizoaffective disorder, where the psychosis of schizophrenia periodically combines with depression.
Until she was 15, Chase was a happy, normal teenager, swimming on her high-school team and singing in their choir. Then the disease took hold, Chase recalls, “Out of nowhere, like a switch had flipped.” While about 80 percent of the risk for schizophrenia is thought to be genetic, Chase has no known family history.
Voices began telling her she was a prophet chosen by Jesus and urging her to be purer to fulfill that role. Chase started wearing white clothing and shunning food and beverages. As she walked around her house at night, she watched dark spirits crawl up the stairs and her own face change shapes in the mirror.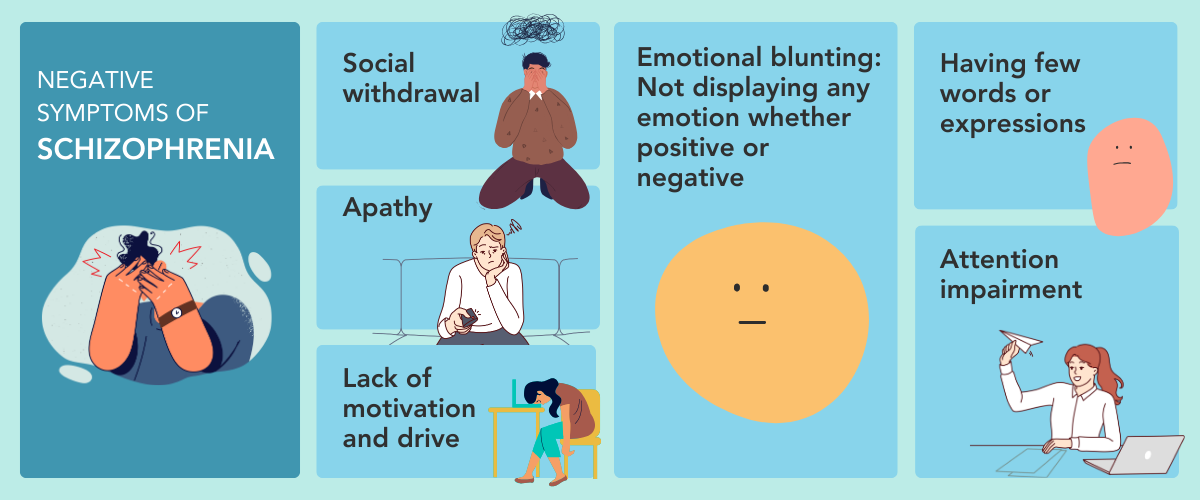
Chase tried to keep the delusional thinking to herself, but within weeks her mother Patricia Stewart became alarmed, especially when Chase wouldn’t take even a sip of water. Stewart whisked her daughter to the hospital, where the pair received the incorrect diagnosis of bipolar 1—also known as manic-depressive disorder—and a prescription for lithium, which is not effective for psychosis.
“I had that title for a long time,” Chase says. It would take 10 years, numerous psychotic episodes, and several hospitalizations before she was properly diagnosed.
Diagnosing women is often hampered by the fact that people suffering delusions don’t recognize them as such. “You don’t go to the doctor and say, I’m having this problem, because insight is impaired,” says Abigail Donovan, director of clinical services for the psychosis program at Massachusetts General Hospital. “It takes people around them to say something is wrong.”
Stewart played that role for Chase. But males may attract more attention from family or teachers because they tend to have more “negative symptoms” such as apathy and withdrawal in addition to the delusions and hallucinations, Donovan says.
Getting an early diagnosis is crucial, since “all the data show the longer the time to good treatment, the worst your prognosis. People with early care get well faster and stay well longer,” Kelly says.
This recognition has sparked several states in recent years to fund First-Episode Clinics specializing in early interventions. (Donovan’s Mass General is one of the original models.) A review published in August found such early, comprehensive treatment is most effective for reducing symptoms and enhancing quality of life.
The role of female hormones
Women also fly under the radar because estrogen has long been known to play a protective role, part of the reason women have a slightly lower rate of illness than men.
With the brain bathed in the hormone following puberty, females who are at risk spend their teenage years establishing relationships and thriving in school. This provides major support when they succumb a few years later, says John Krystal, chair of psychiatry at the Yale School of Medicine. Meanwhile, boys get sick before this crucial social period, a possible reason why males with the disease can be cut off from society and end up on the streets.
But when the protective hormone is withdrawn during menopause, some who avoided earlier psychosis get a later onset. Having a first experience after age 40 is uncommon, but it may include up to 15 percent of the women with schizophrenia—twice the percentage of men who have schizophrenia onset after age 40.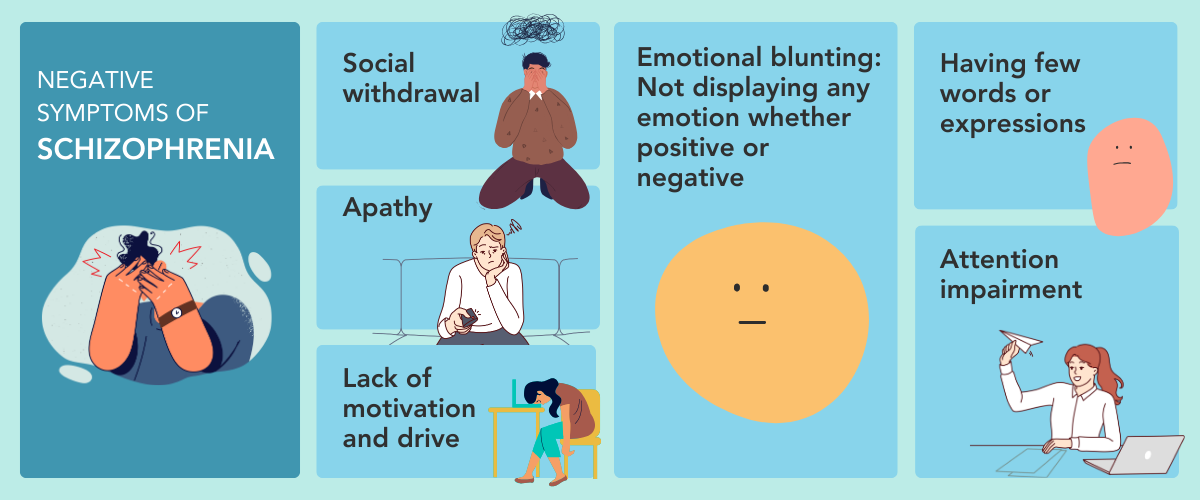
“We don’t know exactly why this happens or what treatments or interventions are best at this age. It’s amazing what an information vacuum there is,” Thakkar says. It’s not even clear that hormones are the only factor behind the midlife bump, since women also experience significant stress during this time—from launching adult children, caregiving older parents, and/or, sometimes, divorce—which is a known trigger for people who are genetically prone, she says.
No unique treatment guidelines have been formulated for women diagnosed in midlife, even though they may respond differently to medications than younger patients and menopausal hormone therapy could potentially help, Thakkar says. She and colleagues are currently enrolling women in a study to begin to answer some of these questions.
Late onset of the disease also warrants unique psychotherapies. “How do we help a child of a midlife woman maintain a close, loving relationship with a parent who may do or say things that don’t make sense? And how do we help the family stay intact and connected?” Donovan asks.
Proper medication is key to women’s success
Even women diagnosed at the more typical, younger ages experience unique issues. One involves the environmental factors that lead to psychosis. Kelly points to physical abuse of girls in childhood, which her research shows later leads to significantly more psychotic symptoms compared to females who were not abused or even to men who were.
Scientists also worry about the impact of cannabis use on the incidence of schizophrenia in teenage girls living in states where the drug has been legalized; this could further shrink the gender gap for schizophrenia rates.
“Cannabis in adolescence is known to increase the probability of expressing psychotic symptoms,” Krystal says. A study in the Lancet published in March found cannabis use among the most predictive for relapse in sufferers.
When it comes to treatments, many common antipsychotics cause more serious side effects in women than men, including hypertension and heart rhythm issues. Some also have a higher rate of one particularly unpleasant side effect—hyperprolactinemia—in which the breasts produce milk and which causes some women to stop taking their medication.
Kelly found the problem can be significantly reduced in women by adding the antipsychotic medication aripiprazole. Findings like these highlight the need for additional gender-specific treatment research, she says.
Disparities also exist when it comes to accessing the most effective schizophrenia drug, clozapine.
The medicine is underprescribed for everyone, experts say, but that’s especially the case for women. In the five years following diagnosis just 27 percent of women were on the drug, according to the Nature study, compared with 31 percent for men.
Psychiatrists hesitate to prescribe clozapine at least in part because of the strict safety requirements imposed by the U.S Food and Drug Administration, known as a risk evaluation and mitigation strategy, or REMS, Kelly says.
FDA requires REMS because clozapine can cause a drop in certain white blood cells, which can lead to severe infections and even death. Doctors who prescribe the drug must order frequent blood tests—weekly for the first six months—if the patient is on it.
Kelly would like to see less frequent blood-monitoring requirements, especially after the first year when the risk drops significantly. This spring, she testified about this alongside Chase before a Congressional committee.
“The risk of dying by suicide [for patients with uncontrolled schizophrenia] is hundreds to thousands of times higher than the risk of dying from low white blood count,” Kelly insists.
Despite Chase seeing numerous psychiatrists following her correct diagnosis, no one offered her clozapine, says Stewart, who is involved in her care. Instead, Chase struggled for years with episodic symptoms and bothersome side effects while on seven successive medications.
Stewart eventually discovered clozapine in an online social media group. When she suggested it to Chase’s physicians, all said no.
“For me as her mother and advocate it was such a struggle to get Analisa on the right medication. How can someone suffering from this disease be expected to advocate for themselves?” Stewart says. Finally, four years ago, after another major psychotic episode and a monthlong hospitalization, Chase was finally put on clozapine.
“I still see things and hear voices sometimes, but now I’m able to separate reality from what’s not real, so I don’t have to engage with it,” Chase says.
Since she began taking the medication, Chase has become stable enough to live on her own, graduate from college, get a part-time job, and enter a healthy romantic relationship. “She’s done incredibly well in spite of her challenges,” Stewart beams.
“Schizophrenia is thought of as a disease where you’re put away, unable to function in society,” Kelly says. Getting the proper diagnosis and treatment upends that trajectory. “Women are living among us, working, and thriving. Some don’t go back exactly to the way they were before," but with the right help they can live meaningful and fulfilling lives.
Source
https://www.nationalgeographic.com/premium/article/schizophrenia-under-diagnosed-women
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4539869/
https://crownviewci.com/blog/schizophrenia-the-misunderstood-disorder/
https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms-causes/syc-20354443#:~:text=Schizophrenia%20is%20a%20serious%20mental,with%20schizophrenia%20require%20lifelong%20treatment.
https://en.wikipedia.org/wiki/Schizophrenia