Sickle Cell Syndrome: Africa's Exclusive Experience
Sickle Cell Syndrome: Africa's Exclusive Experience
Introduction
Sickle cell syndrome (SCS), a genetic blood disorder characterized by abnormal hemoglobin known as hemoglobin S, is a global health issue. However, its impact is most acutely felt in Africa, where it poses significant public health challenges. This article explores the unique experience of African nations with SCS, highlighting the epidemiology, socio-economic implications, healthcare responses, and ongoing efforts to mitigate its impact.
Epidemiology and Prevalence
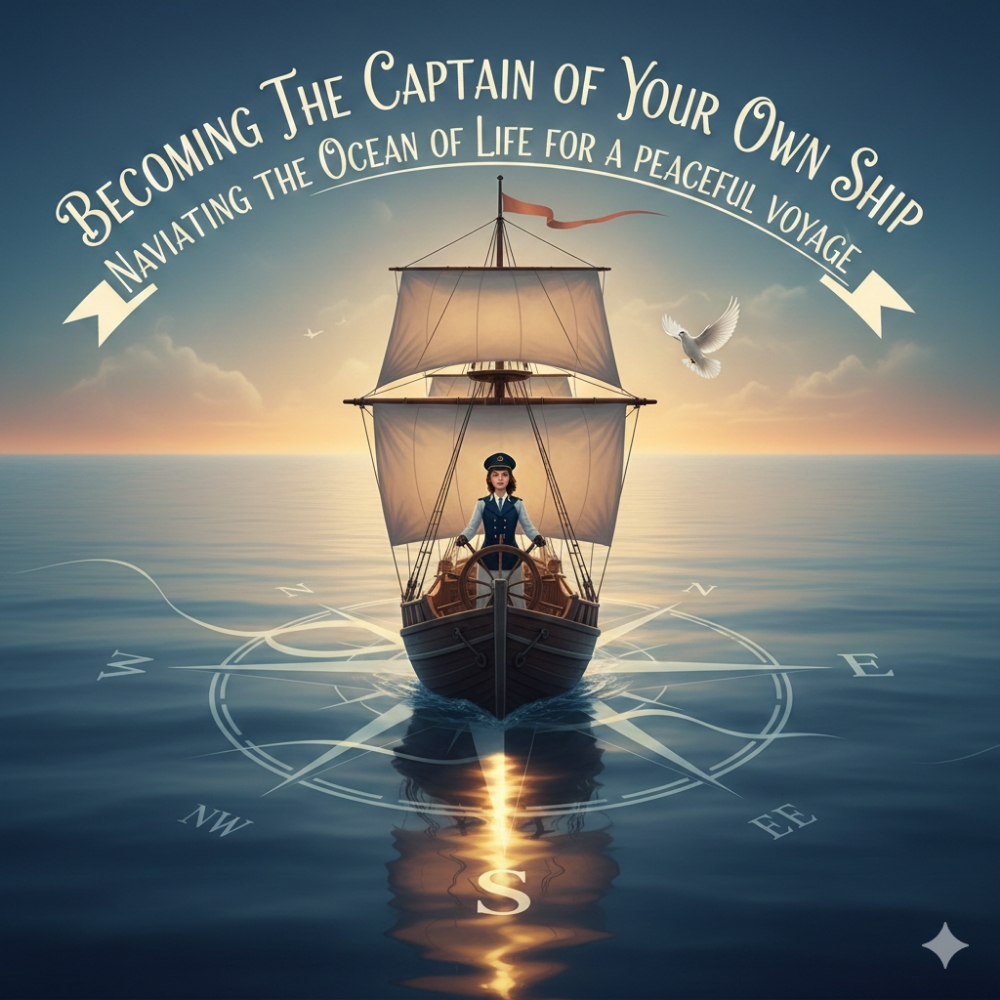
Sickle cell syndrome is most prevalent in sub-Saharan Africa, with the highest frequency in West and Central Africa. Approximately 80% of the global cases of SCS are found on the continent. In some regions, up to 2% of all newborns have the disease, and about 10-40% of the population carries the sickle cell trait. The high prevalence is attributed to a genetic adaptation against malaria; individuals with one sickle cell gene (carriers) have a survival advantage in malaria-endemic areas.
https://www.researchgate.net/figure/The-genetic-map-of-prevalence-of-sickle-cell-disease-in-Africa-44_fig1_303747504
Socio-Economic Impact
The burden of SCS in Africa extends beyond health, impacting socio-economic development significantly. Children with SCS often experience recurrent painful crises, frequent infections, and severe anemia, leading to missed school days and reduced educational attainment. Adults face challenges in maintaining consistent employment due to health complications. The economic burden on families is substantial, as they often bear the cost of treatment and care, leading to financial instability .
Healthcare Challenges
The healthcare infrastructure in many African countries is ill-equipped to manage SCS effectively. There are several barriers to care, including limited access to comprehensive healthcare services, lack of specialized medical professionals, and inadequate diagnostic facilities. Many patients are diagnosed late, and preventive care and routine management are not widely available. Moreover, the stigma associated with the disease can prevent families from seeking timely medical intervention .
Efforts and Interventions
Recognizing the severity of SCS, various African governments, non-governmental organizations, and international bodies have initiated programs to address the disease. Key interventions include:
1. Newborn Screening Programs: Early diagnosis through newborn screening is crucial for managing SCS. Countries like Ghana and Nigeria have initiated pilot programs to screen newborns, enabling early intervention and better outcomes .
2. Public Awareness Campaigns: Educating communities about SCS is vital to reduce stigma and encourage early treatment. Campaigns focus on dispelling myths, promoting genetic counseling, and advocating for regular medical check-ups .
3. Access to Care and Treatment: Efforts are underway to improve access to affordable care. This includes the provision of essential medications like hydroxyurea, pain management therapies, and blood transfusions. Some regions have established specialized sickle cell clinics to provide comprehensive care.
4. Research and Partnerships: Collaborative research efforts aim to understand the disease better and develop new treatments. International partnerships with institutions in Europe and the United States have facilitated advancements in genetic research and therapeutic interventions .
Conclusion
Sickle cell syndrome remains a pressing health challenge in Africa, with profound implications for affected individuals and their communities. Despite the significant obstacles, ongoing efforts to improve diagnosis, treatment, and awareness offer hope. Continued investment in healthcare infrastructure, education, and research is essential to alleviate the burden of SCS in Africa and ensure better health outcomes for future generations. The collective action of governments, organizations, and communities is crucial in turning the tide against this debilitating disease
References
1. [WHO | Sickle Cell Disease](https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease)
2. [Centers for Disease Control and Prevention | Sickle Cell Disease](https://www.cdc.gov/ncbddd/sicklecell/data.html)
3. [Bainbridge, R. S., et al. "The socio-economic burden of sickle cell disease in Africa." *Journal of Health Economics* (2020)]
(https://www.sciencedirect.com/science/article/abs/pii/S0167629619303727)
4. [Makani, J., et al. "Health care costs and access to care for patients with sickle cell anemia in Tanzania." *The Lancet* (2011)](https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(11)60355-2/fulltext)
5. [Piel, F. B., et al. "Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates." *The Lancet* (2013)](https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)61232-3/fulltext)
6. [Akinyanju, O. O., et al. "Managing sickle cell disease in low-income countries." *British Journal of Haematology* (2005)](https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2141.2005.05615.x)
7. [Ohene-Frempong, K., et al. "Newborn screening for sickle cell disease in Ghana." *Pediatric Blood & Cancer* (2008)](https://onlinelibrary.wiley.com/doi/full/10.1002/pbc.21401)
8. [Nnodu, O. E., et al. "Implementing newborn screening for sickle cell disease as part of immunization programmes in Nigeria: a feasibility study." *The Lancet* (2010)](https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)60201-5/fulltext)
9. [McGann, P. T., et al. "A decade of newborn screening for sickle cell disease: lessons learned and future directions." *Pediatrics* (2015)](https://pediatrics.aappublications.org/content/136/6/e1492)
10. [WHO | Sickle Cell Disease: A strategy for the WHO African Region](https://www.afro.who.int/publications/sickle-cell-disease-strategy-who-african-region)
11. [Tshilolo, L., et al. "Hydroxyurea for children with sickle cell anemia in sub-Saharan Africa." *The New England Journal of Medicine* (2019)](https://www.nejm.org/doi/full/10.1056/NEJMoa1813598)
12. [Bolaños-Meade, J., et al. "Blood transfusions in sickle cell disease: evidence from a multicenter randomized clinical trial." *Journal of the American Medical Association* (2020)](https://jamanetwork.com/journals/jama/fullarticle/2767931)
13. [Archer, N., et al. "Genetic therapies in sickle cell disease: A systematic review and meta-analysis." *The Lancet Haematology* (2021)](https://www.thelancet.com/journals/lanhae/article/PIIS2352-3026(21)00019-3/fulltext)
14. [DeBaun, M. R., et al. "Collaborative research networks in sickle cell disease: the road ahead." *Blood* (2016)](https://ashpublications.org/blood/article/127/7/798/34750/Collaborative-research-networks-in-sickle-cell)