How the Microbiome Affects Mental Health
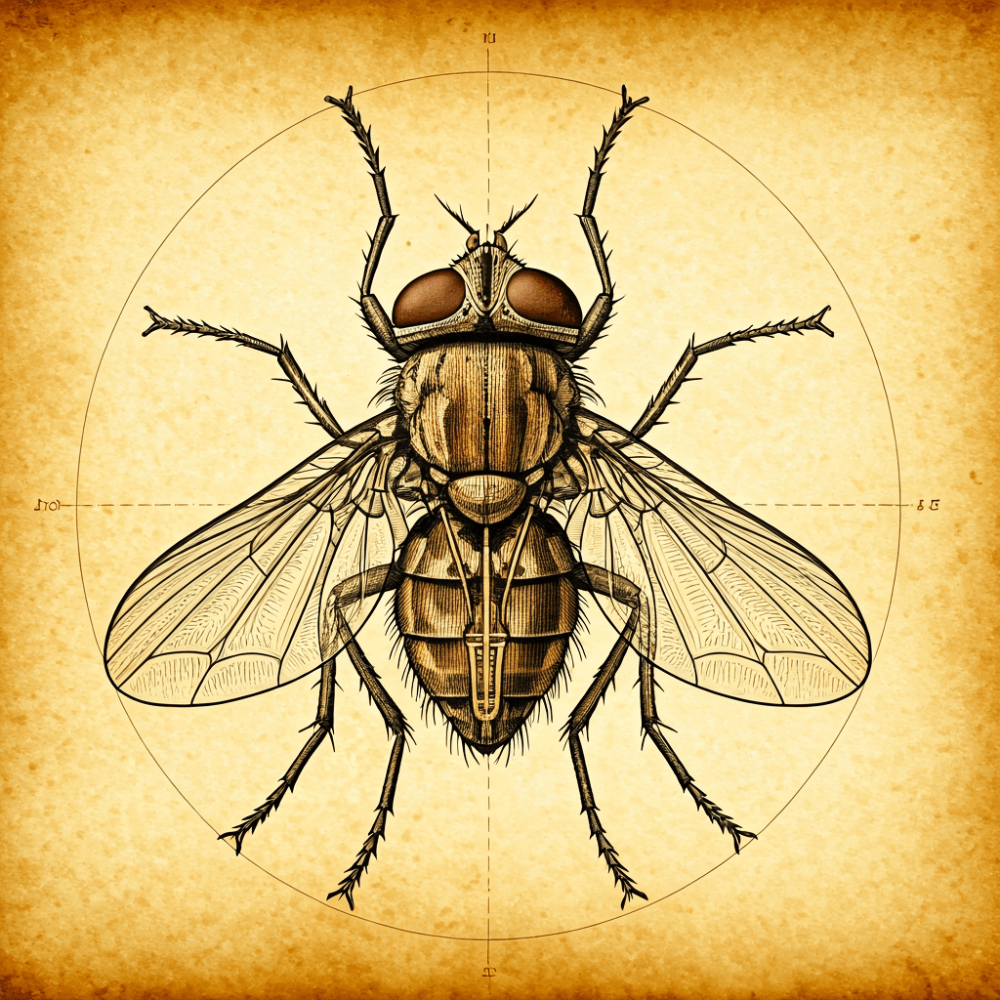
The link between our gut and mental health is increasingly drawing the attention of researchers and healthcare professionals alike. Often called the “second brain,” the gut is now recognized as a dynamic environment that communicates with the brain, influencing everything from mood and cognition to stress responses. This relationship pivots on the microbiome the community of trillions of bacteria, fungi, and viruses that reside in our digestive system.
Through biochemical signals, these microscopic organisms have a significant impact on our mental well-being, shedding light on promising avenues for mental health treatment.
The Microbiome-Gut-Brain Axis
The microbiome-gut-brain axis is the communication pathway that connects our central nervous system to the gut. It operates through complex biological channels involving the immune system, hormonal signals, and neurotransmitters.
This intricate network underscores why an imbalance in the gut microbiome, often termed “dysbiosis,” is associated with various mental health disorders, including anxiety, depression, and even neurodevelopmental conditions.
- Immune System Activation: The microbiome plays a critical role in regulating immune responses, which in turn can impact inflammation. Persistent inflammation can lead to neuroinflammation, a factor linked to mental health disorders such as depression.
- Hormonal Pathways: The gut microbiome influences the hypothalamic-pituitary-adrenal (HPA) axis, which controls the body’s response to stress. A dysregulated HPA axis is often observed in individuals with anxiety and depression.
- Neurotransmitter Production: Bacteria in the gut produce neurotransmitters such as serotonin, dopamine, and GABA, essential for mood regulation and mental stability.
Through these pathways, a well-balanced microbiome has the potential to protect mental health, while dysbiosis can disrupt these functions and contribute to psychological disorders.
Impact of Gut Dysbiosis on Mental Health
Dysbiosis, or the imbalance of microbial populations, is closely tied to several mental health challenges. Factors contributing to gut dysbiosis include a poor diet, chronic stress, lack of exercise, antibiotic use, and environmental toxins.
When the diversity and balance of the gut microbiome are compromised, the communication between the gut and the brain is disrupted, resulting in potential changes in mood, behavior, and cognitive function.
- Mood Disorders: Research reveals that individuals with major depressive disorder (MDD) often have lower levels of beneficial gut bacteria, such as Lactobacillus and Bifidobacterium. These bacteria are crucial in regulating serotonin production—a neurotransmitter that influences mood and happiness.
- Anxiety Disorders: Dysbiosis may trigger heightened stress responses, particularly through the HPA axis, increasing susceptibility to anxiety disorders. Studies have found that people with generalized anxiety disorder (GAD) often display altered gut microbiomes compared to healthy individuals.
- Cognitive Impairment: Emerging research suggests that gut dysbiosis may be linked to neurodegenerative diseases such as Alzheimer’s. Inflammatory processes triggered by a compromised microbiome can affect brain function, impacting memory and cognition.
By exploring the relationship between dysbiosis and mental health, researchers are uncovering new pathways for addressing psychological disorders through targeted microbiome interventions.
Therapeutic Potential of Microbiome Modulation
Recognizing the microbiome’s influence on mental health has paved the way for innovative therapeutic strategies. Through dietary adjustments, probiotics, and prebiotics, individuals can enhance their microbiome, potentially improving their mental well-being. Here are several promising avenues in microbiome modulation:
- Probiotics and Prebiotics: Probiotics live bacteria supplements—can restore beneficial bacterial populations, while prebiotics (dietary fibers that promote healthy bacteria growth) serve as their fuel. Studies show that specific probiotic strains, such as Lactobacillus helveticus and Bifidobacterium longum, may alleviate symptoms of anxiety and depression.
- Dietary Interventions: The gut microbiome thrives on a fiber-rich diet, with foods like vegetables, whole grains, and fruits fostering bacterial diversity. Additionally, omega-3 fatty acids, found in fish and flaxseeds, support gut health and may improve cognitive function.
- Fecal Microbiota Transplant (FMT): FMT involves transferring gut bacteria from a healthy donor to someone with a compromised microbiome. Although primarily used for severe infections, FMT shows promise in alleviating mood disorders by restoring microbial balance.
- Psychobiotics: The term “psychobiotics” refers to probiotics that have been shown to positively affect mental health. Research suggests these bacteria can reduce cortisol levels (the primary stress hormone) and enhance resilience to stress.
Incorporating these approaches offers a multifaceted strategy to address mental health by optimizing the gut microbiome, reflecting a shift toward more integrative and personalized treatments.
The Future of Microbiome-Based Mental Health Interventions
Advances in microbiome research are rapidly expanding our understanding of mental health, with promising implications for future treatments. As science uncovers the genetic diversity within the microbiome and how it changes over time, the potential for targeted therapies will continue to grow.
- Personalized Medicine: Advances in genomic and microbiome sequencing are paving the way for personalized medicine. Individuals could receive specific probiotic strains or dietary plans tailored to their unique microbiome profile, potentially transforming mental health treatment.
- Biomarker Identification: The identification of microbiome-related biomarkers may aid in diagnosing mental health conditions earlier, allowing for preventive measures or targeted interventions before symptoms escalate.
- Pharmaceutical Development: As we learn more about how certain bacteria produce mood-enhancing compounds, pharmaceutical companies may develop drugs that mimic or amplify these effects, offering an entirely new class of antidepressants or anxiolytics.
With these emerging opportunities, the microbiome is set to play a pivotal role in the future of mental health care. Recognizing the power of the gut-brain connection could lead to a more holistic approach to mental well-being, where nurturing our microbiome becomes as essential as traditional mental health practices.
Conclusion
Understanding the intricate connection between the microbiome and mental health opens up transformative avenues for treatment and well-being. Through the microbiome-gut-brain axis, our gut bacteria have a profound impact on mood, cognition, and resilience. As research progresses, we can expect an era of more personalized and microbiome-focused mental health care, where diet, probiotics, and even advanced therapies like psychobiotics become integral to supporting our mental health. By optimizing the microbiome, we gain a powerful tool to enhance not only our physical health but our psychological resilience, enriching the quality of life in previously unimaginable ways.
Sources
- Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behavior. Nature Reviews Neuroscience.
- Foster, J. A., Rinaman, L., & Cryan, J. F. (2017). Stress & the gut-brain axis: regulation by the microbiome. Neurobiology of Stress.
- Mayer, E. A., Knight, R., Mazmanian, S. K., Cryan, J. F., & Tillisch, K. (2014). Gut microbes and the brain: paradigm shift in neuroscience. The Journal of Neuroscience.
- Rieder, R., Wisniewski, P. J., Alderman, B. L., & Campbell, S. C. (2017). Microbes and mental health: a review. Brain, Behavior, and Immunity.
- Valles-Colomer, M., et al. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology.
- Dinan, T. G., & Cryan, J. F. (2013). Melancholic microbes: a link between gut microbiota and depression? Journal of Psychiatric Research.
- Yano, J. M., et al. (2015). Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell.
- Dash, S., Clarke, G., Berk, M., & Jacka, F. N. (2015). The gut microbiome and diet in psychiatry: focus on depression. Current Opinion in Psychiatry.
- Johnson, K. V., & Foster, K. R. (2018). Why does the microbiome affect behavior? Nature Reviews Microbiology.
- Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology.